Have you ever experienced deep, aching pain in your bones or joints that doesn’t seem to go away? It might not just be regular soreness—it could be a sign of bone marrow edema (BME).
BME is a condition where excess fluid builds up inside the bone marrow, leading to inflammation and discomfort. It’s often linked to injuries, arthritis, or underlying medical conditions. While it may sound concerning, early diagnosis and proper treatment can significantly improve symptoms and prevent long-term complications.
In this guide, we’ll explore what bone marrow edema is, its causes, and symptoms, how doctors diagnose it, and the best treatment options available. Whether you’re experiencing bone pain or just want to learn more, this blog will provide valuable insights into managing and preventing BME effectively.
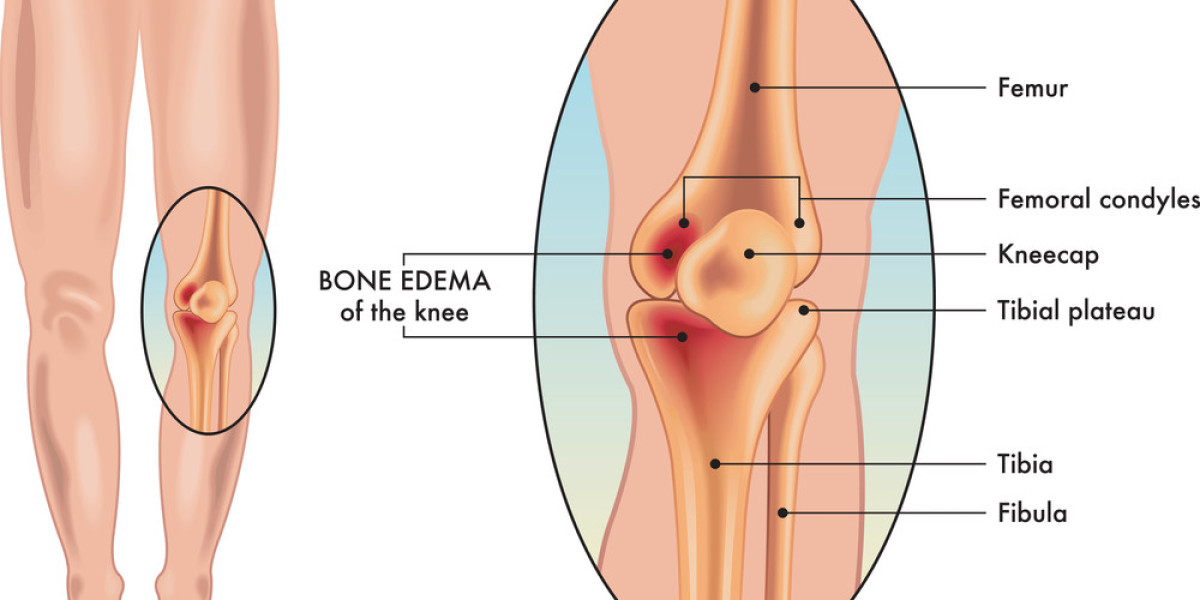
What Exactly Is Bone Marrow Edema?
Bone marrow is the soft, spongy tissue inside bones that produces blood cells and stores fat. When fluid accumulates in this area, it results in bone marrow edema, causing pain, stiffness, and swelling.
This condition is most commonly detected through MRI scans and is associated with various health issues, including:
Injuries (such as fractures or repetitive stress on bones)
Arthritis (like osteoarthritis and rheumatoid arthritis)
Medical conditions (osteonecrosis, cancer, infections)
Many people confuse BME with conditions like osteoporosis or bone fractures, but it’s different. BME is a temporary condition caused by fluid accumulation, whereas osteoporosis involves long-term bone weakening.
What Causes Bone Marrow Edema?
Bone marrow edema can develop for various reasons. Understanding the causes can help in both prevention and treatment.
1. Injuries & Trauma
A common trigger for BME is physical injury. This can include:
Fractures: A broken bone can lead to swelling inside the bone marrow.
Stress Injuries: Runners and athletes often experience stress fractures that result in BME.
Repetitive Strain: Overuse of joints—common in sports or heavy physical labor—can contribute to the condition.
2. Arthritis & Inflammation
Chronic joint conditions can also lead to BME:
Osteoarthritis: The wearing down of cartilage can cause inflammation in the bone marrow.
Rheumatoid Arthritis: An autoimmune condition where the immune system attacks joints, leading to fluid buildup.
Spondyloarthritis: A form of arthritis affecting the spine and large joints.
3. Medical Conditions
Certain diseases can contribute to bone marrow edema, including:
Osteonecrosis: A condition where bone tissue dies due to lack of blood supply.
Bone Infections: Bacterial infections like osteomyelitis can lead to fluid accumulation.
Cancer: Bone tumors or metastatic cancer can cause localized BME.
4. Post-Surgical Effects
After joint or orthopedic surgeries, some patients develop temporary BME as the body responds to trauma. While this typically resolves on its own, it may require monitoring.
Recognizing the Symptoms: When Should You Be Concerned?
Bone marrow edema symptoms vary depending on the cause and severity. However, some key signs to watch for include:
1. Persistent Pain
Pain is the most common symptom of BME. It can feel deep, aching, or throbbing and often worsens with activity.
2. Swelling & Stiffness
Affected areas may become swollen, leading to reduced joint mobility. This is especially noticeable in weight-bearing bones like the knees, hips, or ankles.
3. Hidden Symptoms
Some people may also experience:
Fatigue due to chronic pain and inflammation.
Weakness in the affected limb, making daily activities more challenging.
4. When to See a Doctor
Seek medical attention if:
Pain persists for weeks without improvement.
Swelling and stiffness worsen over time.
You experience severe discomfort while walking or moving joints.
Diagnosing Bone Marrow Edema: How Do Doctors Identify It?
Early detection of BME is crucial for effective treatment. Doctors use a combination of medical history, imaging, and physical examinations to diagnose it.
1. MRI Scans – The Gold Standard
MRI (Magnetic Resonance Imaging) is the most reliable tool for diagnosing BME. It can detect fluid buildup even before visible damage appears on X-rays.
2. X-rays & CT Scans
While X-rays do not show BME directly, they help rule out fractures or other bone conditions. CT scans may be used if detailed imaging is required.
3. Physical Examination & Symptoms Assessment
Doctors will evaluate your pain, swelling, and movement limitations to determine whether further imaging tests are needed.
Treatment Options: What Can Be Done?
The right treatment for BME depends on its cause and severity. Here are some common approaches:
1. Rest & Activity Modification
Reducing physical stress on affected bones is key to recovery.
Using crutches, braces, or orthopedic support can help reduce pressure.